August 20, 2019
Should Doctors Make Less Money?
 In an August 1st commentary published in the Washington Post, columnist Catherine Rampell asks an intriguing question of the Democratic presidential candidates promoting a Medicare-for-All health insurance program: “Will your plan require doctors to make less money?” Rampell believes the issue of physician compensation is the “real third rail of healthcare reform.”
In an August 1st commentary published in the Washington Post, columnist Catherine Rampell asks an intriguing question of the Democratic presidential candidates promoting a Medicare-for-All health insurance program: “Will your plan require doctors to make less money?” Rampell believes the issue of physician compensation is the “real third rail of healthcare reform.”
After eliminating other healthcare budget busters (greedy insurers, ridiculously high administrative costs, ridiculously high drug costs), Rampell reveals an obvious truth: Americans simply pay more for healthcare services than people in other advanced economies. For emphasis, she references economist Uwe Reinhardt’s shorthand explanation for America’s high healthcare costs, “It’s the prices stupid!”
In Rampell’s assessment, presidential candidates promoting Medicare-for-all confront an unpalatable dilemma: either pay doctors significantly less money (like they do in Canada) and risk system-wide disruption; or continue paying doctors at current levels which makes any Medicare-for-All plan vastly more expensive.
She concludes with this piercing observation, “But either way, candidates have to make a choice about a question that is fundamental to understanding what their plans would do, and whether they add up. So far, they haven’t.”
Here’s the rub. Rampell’s analysis is inadequate because it fails to recognize that medical practices themselves are a principal contributor to healthcare’s soaring costs.
America’s pluralistic healthcare system is an intricate dance between medical practices and payment for medical services. Consequently, payment for medical services influences the delivery of those services in good and bad ways:
- Good medical practices deliver appropriate, personalized, convenient and efficient healthcare with full transparency regarding outcomes, quality, costs, prices and consumer experience.
- Bad medical practices perpetuate inappropriate, institutionalized and high-cost healthcare through billing complexity, market concentration and/or lack of transparency.
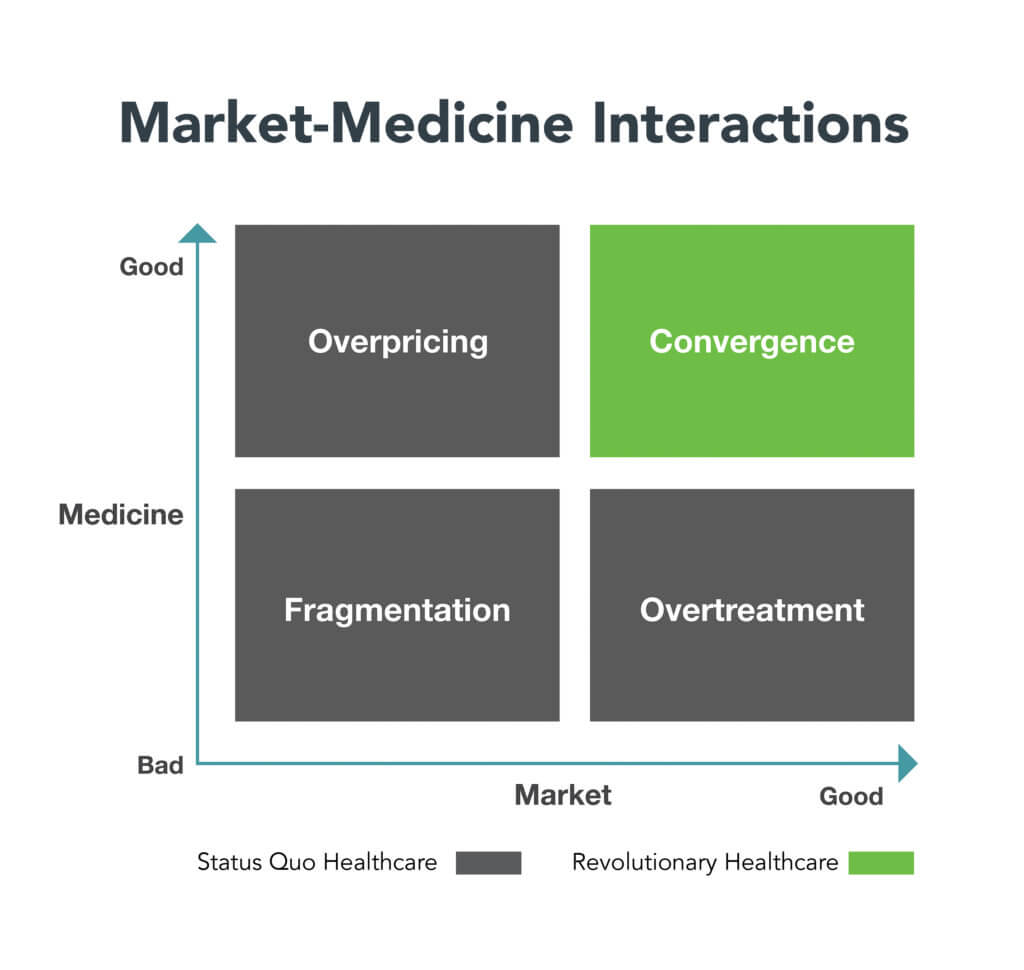
Markets also exhibit good (competitive) and bad (anticompetitive) behaviors. The matrix below illustrates the characteristics of good and bad market-medicine interactions.
FRAGMENTATION, OVERPRICING AND OVERTREATMENT
The conjunction of bad medical practices and bad market behaviors (Fragmentation) is destructive and dangerous. It leads to fragmented, overpriced care delivery that is mistake-prone and ignores consumer needs.
Fragmented healthcare includes hospitals that overcharge for routine services and neglect patients; disconnected outpatient clinics; rogue ERs that generate surprise bills; surgical units that work banker’s hours despite urgent, 24/7 demand. These practices riddle American healthcare. They diminish quality, ignore customer service and waste societal resources.
Mispriced good medicine (Overpricing) is wasteful by definition. An MRI may be necessary, but it’s wildly overpriced at $5000. Bad medicine that is competitively priced (Overtreatment) is ineffective, unnecessary and may cause harm to patients. An unnecessary MRI is wasteful even if it only costs $500.

Fragmentation, Overpricing and Overtreatment are the three faces of “Status Quo Healthcare.” They thrive in opaque and unaccountable operating environments. Healthcare’s waste and unsustainable costs originate here. The American people deserve better. They should expect great healthcare at fair prices.
Individualized and holistic care services within efficient markets (Convergence) epitomize “Revolutionary Healthcare.” By definition, Revolutionary Healthcare is pro-market, not pro-business. It reinforces level-field competition, transparency and accountability. It consistently and relentlessly delivers value to consumers.
There are pockets of Revolutionary Healthcare in America today. They include companies that provide expert second opinions, fixed-priced surgeries, timely telemedicine services and convenient low-cost MRIs. Pro-market health companies deliver the right care at the right time in the right place at the right price. That’s healthcare as it should be.
The other fundamental flaw with Rampell’s logic is that she ignores the power of “defense” to reduce acute interventions. Preventing a surgery is a better outcome than having the most advanced surgery by the most accomplished surgeon in the most modern facility.
As Alabama football coach Bear Bryant famously observed, “Offense sells tickets. Defense wins championships.” Contrary to Bryant’s wisdom, Status Quo Healthcare operates high-octane offenses and neglects defense. It “sells tickets” to maximize the volume of high-margin treatments. It underinvests in community health.
In contrast, Revolutionary Healthcare plays defense superbly. It invests in health promotion, disease prevention, chronic disease management, dental care and mental health services. It pays for these added frontline services by disinvesting in unnecessary and/or overpriced procedures and tests.
Revolutionary Healthcare treats the whole person. It provides appropriate, timely and convenient care. It engages consumers. It’s kind and compassionate. It applies smart technologies. It “wins championships.”
So here’s the answer to Rampell’s original question. Doctors who deliver better care with great service at competitive prices will earn more money. Those that don’t will earn less. That’s the American way.
In Revolutionary Healthcare, outcomes matter, customers count and value rules.





