August 10, 2020
No Time to Waste: COVID-19 Is Propelling Operational Transformation in Health Systems
Boxer Mike Tyson famously observed, “Everyone has a plan until they’re punched in the face.” COVID-19 knocked America’s healthcare system to the canvas. Even as hospitals expanded critical care capacity to treat COVID-19 patients, a dramatic drop in elective surgeries wreaked financial havoc on providers large and small.
Operating losses are in the billions and rising. Health systems confront enormous uncertainty as they try to return to normalized operations.
How individual health systems respond now will determine their ability to compete in the future, within an evolving healthcare marketplace that rewards agility, efficiency, responsiveness and safety. In particular, systems with a bias for action, that pursue newfound opportunities resulting from the reemergence of operational excellence, will emerge stronger than ever. Opportunity abounds, but there is no time to waste.
Pandemic Disruption
While the COVID-19 surge has overwhelmed critical capacity in some markets, nationwide efforts to contain the pandemic through lockdowns have stressed the U.S. healthcare system in multiple ways. Costs are up, revenues are down. Health system staff have faced the extremes of layoffs or intense overwork treating COVID-19 patients. The quality of patient care has suffered.
Under pressure, hospitals paid premium prices for PPE, vital equipment (e.g., ventilators) and temporary clinical workers to cover surge periods. Federal payments to offset operating losses, fund COVID-19-related care, and pay for virtual care visits have mitigated some of the financial impact.
Overall revenues are down due to a dramatic decline in elective procedures, chronic care, screening and preventative care appointments. Even patients requiring emergency care are avoiding hospitals, clinics or emergency rooms in breathtaking numbers. To offset the revenue losses, health systems have delayed capital investment, laid off or furloughed workers and squeezed suppliers.
Times are hard. 1.4 million healthcare workers lost their jobs in April during the nation’s greatest healthcare crisis in over a century. Already high stress levels are increasing.
Patient health has suffered as well, with the lack of access to disease management and treatment and the avoidance of preventative health measures. In April, Beth Israel experienced a 60% decline in referrals for breast, blood and hematologic cancers. The American Academy of Pediatrics estimates that up to 40 percent of children scheduled for vaccinations in spring 2020 have missed them. Deferring vital screening tests and preventative care for a prolonged period will contribute to more unnecessary deaths in the months and years to come.
While the first half of 2020 was catastrophic for health systems, the second half of 2020 could be even worse. With the relaxation of shelter in place policies, hospitals in some states are seeing a resurgence of COVID-19 cases. In other regions, systems are scrambling to recover lost volume. As hospitals seek a return to normalcy, uncertainty reigns.
Profound questions remain unanswered:
- How can we restore elective surgeries?
- Will patients return?
- Will there be a surge in sick patients who have delayed care?
- Will social distancing need to be reinstated to avoid resurging waves of COVID-19?
- How will COVID-19 intersect with seasonal influenza this fall and winter?
- How will these dynamics vary geographically?
- Will COVID-19 mutate and become more or less virulent?
- When will a vaccine be available and how effective will it be?
This period of strategic uncertainty is likely to last for the foreseeable future. COVID-19 has upset, perhaps permanently, traditional demand patterns for acute care services. It also is upending traditional mindsets and cultural conventions.
Newfound Bias for Action
Former Chicago Mayor Rahm Emanuel famously advises leaders to “never waste a crisis.” Periods of crisis create opportunities to accelerate transformative change. Enlightened health system leaders are embracing this mindset, implementing strategies to not only address short-term, supply-demand imbalances, but also create a long-term competitive advantage. They are aggressively pursuing digital solutions and productivity improvements.
In health systems across the country, leaders marvel at the levels of transformative change they have implemented since March. To continue care during the first few months of COVID-19, health systems and care organizations expanded virtual care capacities and implemented new ways to engage with consumers digitally. To manage COVID-19 patient capacity, they’ve streamlined care transitions within their walls, and found creative solutions for patients outside their walls.
Moreover, healthcare’s supply-demand dynamics are changing in real time. Based on an April consumer survey, the PwC’s Health Research Institute estimates that more than 16 million consumers used telehealth for the very first time during the pandemic’s first month. That was just the beginning.
Health systems are experimenting with new delivery models, exploring strategic partnerships, and unleashing professionals to practice at the top of license.
Jonathan R. Slotkin, Karen Murphy and Jaewon Ryu from Geisinger Health Systems capture the infectious spirit that permeates enlightened management teams in a recent Harvard Business Review article.[1]
“Now is the time to boldly transform our health care systems in ways we have previously been unable to. We should use this unprecedented opportunity to fix what hasn’t worked and direct our full attention to new and greater goals centered on creating value for patients.”
There really is no time to waste.
Operational Excellence in the Next Normal
One of the biggest opportunities to innovate and create value is in healthcare operations. This may come as a surprise to some. While improving operational efficiencies has been a persistent goal for many organizations, past efforts have seldom delivered sustained gains. Once managers shift attention to a new problem, operations revert back to their prior state — manual, inefficient, and variable.
As a result, even in the best of times many health systems struggle to deliver efficient patient flow. All too often, they rely on the heroic actions of frontline providers to keep the system running, which results in high levels of burnout.
Fortunately, new advances in artificial intelligence, machine learning, and behavioral science enhance the ability of health systems to tackle long-standing operational challenges. Game-changing strategies accelerate throughput and improve the system-wide ability to recognize and respond to quickly shifting conditions.
New technologies for real-time operations enable leaders to deliver and sustain operational improvements by providing three interrelated capabilities:
- They enable teams to identify issues — in the past, present, and future, predicting bottlenecks before they occur. Key technologies include AI, ML, and in the era of COVID-19, epidemiological models for predicting case volumes and the impact on critical hospital resources.
- They help frontline teams orchestrate actions to address or avoid operational issues by hardwiring standard work, facilitating collaboration among teams and ancillaries, and automating repetitive tasks. For this capability, technologies for habit formation, collaboration, and automation are all essential.
- They enable leaders to manage accountability, providing escalation pathways and root cause analyses. This requires AI, real-time communications and statistical outcomes analyses.
Delivering Short-and Long-Term Value
These new technologies for automated operations can address many of the challenges currently facing health systems, delivering both short- and long-term benefits, including:
Increased Revenues: Reducing length of stay enables faster throughput, which enables hospitals to treat more patients within equivalent time frames. More treatments translate into more revenues under transaction-based payment models. Importantly, higher case throughput increases the supply of medical-surgical beds available for elective surgeries, the most profitable component of hospital services.
Decreased Costs: Hospitals currently without capacity constraints still benefit from shorter length of stay. LoS reduction results in fewer excess days and lower variable costs. Combined with increasing per-unit revenues, decreasing per-patient treatment costs positions hospitals to operate closer to profitability at Medicare payment rates, an increasingly important success metric.
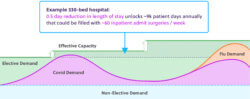
Additional Effective Capacity: During the initial phases of COVID-19, health officials and provider organizations focused on “flattening the curve” to bring demand for critical care beds in line with regional capacity. Reducing length of stay for both Med-Surg and ICU beds works on the other side of the equation, “raising the bar” and increasing effective capacity. Some analyses suggest that a 0.5 day decrease in LOS can unlock approximately 75% of the capacity required for COVID-19-related demand. Unlike the creation of new physical capacity, effective capacity does not require incremental funding and additional staff.
Reduced Burden on Frontline Teams: Making real-time decisions with incomplete information is always challenging for frontline teams, and even more so in a crisis. Using real-time data, background algorithms can apply predictive modeling to help teams make challenging decisions. For example, a smart automated system can quickly identify patients ready to step down from ICU and deliver this information to frontline staff via behavioral nudges. Intelligent systems relieve the cognitive burden on frontline teams and can automate low-level and time-consuming manual tasks so clinicians practice to the top of their license.
Improved Management Decisions: Improving care delivery at the point of care is essential but not sufficient to optimize hospital throughput. Management must understand the entirety of clinical operations to allocate resources effectively, intervene where units falter and anticipate volume surges that could overwhelm routine operations.
Operational intelligence can enable scenario planning for COVID-19 demand, e.g. assessing the impact of social distancing measures, elective surgery strategies and PPE consumption. Automated escalations can self-correct the way an ICU or med-surg unit is functioning. Machine learning using real-time public and hospital data can anticipate and prepare for volume surges. Hospitals can run sophisticated statistical analyses and dig into root causes to drive continuous performance improvement.
Enhanced Patient Care: Better scenario planning enables hospitals to set and manage patient expectations in accordance with anticipated volume and service demands. Better frontline decision making results in less care variation and more consistent care outcomes. Reduced length of stay reduces the risk of complications and hospital-acquired infections. It also frees staff to engage with patients and their families, provide emotional support and win their trust.
By acting now to address COVID-19 challenges today, health systems are developing capabilities to manage and operate acute facilities more effectively and efficiently tomorrow.

Achieving Medicare-Breakeven Performance
These benefits combine to help health systems address the ongoing challenge of margin erosion. Before COVID-19, health systems were already confronting significant margin pressures. In recent years the Congressional Budget Office projected that 40%-50% of hospitals could have negative margins by 2025.
New risk-based payment models, more demanding buyers of healthcare services and pro-market regulatory changes intensify that pressure. Already frightened by healthcare costs, consumers are choosing new delivery models or foregoing care.
As the population ages, the payer mix has been shifting from high-margin commercial coverage to much lower-margin governmental coverage. Together, these forces are spurring healthcare leaders to pursue a path towards operating their businesses at Medicare breakeven margins.
COVID-19 has exacerbated margin pressures in two ways. First, health systems have had to replace high-margin elective surgeries with lower-margin COVID-19 patients. And secondly, higher levels of unemployment have resulted in more people joining Medicaid and/or becoming uninsured, accelerating the payment mix shift toward higher percentages of lower-paying, governmentally-insured patients.
In this environment, operational improvements that increase revenues and decrease costs are enormously valuable. For example, multi-hospital systems can typically expand margins by tens of millions of dollars per year by eliminating Medicare excess days, backfilling the newly created capacity, and better anticipating and managing surges in volumes.
Once theoretical strategies for improving operations are becoming common practice and achieving breakthrough results. Real-time operations adapt capacity and facilities to treat the influx of very sick COVID-19 patients. They also help prepare for surges in delayed care and new wave of COVID-19 patients. Throughout, real-time operations power performance improvement initiatives to support growing value-based care delivery.
This is what M Health Fairview was able to accomplish in partnership with Qventus. Through real-time operations, present and future care delivery have come together in remarkable fashion.
COVID-19 Care at M Health Fairview
M Health Fairview, a 13-hospital system based in Minnesota, partnered with Qventus in 2018 to optimize patient flow across the health system. The Qventus platform has enabled the organization to decrease length of stay, increase discharges before 11am, and streamline ED operations. In 2019, the company launched a System Operations Center (SOC), an enterprise-wide operational command center that coordinates patient flow across the system’s 2,100+ beds.
When COVID-19 emerged, M Health Fairview’s leadership urgently needed system-wide visibility into respiratory resources, ICU capacity, and other critical, distributed resources. Qventus’ advanced scenario planning models predicted a rapid increase in hospitalizations in the region.
Recognizing the need to develop a pandemic strategy that went well beyond efficient utilization of beds, M Health Fairview established an Incident Command Center at SOC and selected units within each hospital for treating COVID-19 patients.
Qventus increased SOC’s situational awareness and generated AI-driven interventions that identified opportunities to increase M Health Fairview’s critical care capacity. Within days, Qventus tools provided real-time visibility into negative airflow rooms, ventilators, and ICU beds throughout the company’s health system. M Health Fairview’s Director of Inpatient Operations, Mary Jo Huppert, describes the tool’s effectiveness as follows,
“With Qventus, we have global transparency into our respiratory resources and ICU capacities to help us effectively address COVID needs as a system. We see where surges are developing at the different sites and can quickly redirect patient demand within the system.”
With COVID-19 threatening to overwhelm its care capacity, M Health Fairview needed to relieve pressure in its ICUs and create new capacity within its Med-Surg units. To address these challenges, Qventus provided AI-based recommendations for transferring ICU patients and discharging patients in Med-Surg units. These recommendations include potential bottlenecks and suggestions for addressing them.
Using real-time automated “nudges” to make smarter point-of-care decisions, the SOC freed up ICU and Med-Surg beds. It also created “effective” bed capacity to meet additional COVID-19 demand. People and intelligent operational systems aligned within M Health Fairview to create needed capacity without crushing an already-burdened frontline staff.
“In a disaster, people lose the time they need to think. And patient flow, which is always a problem, becomes especially critical,” said Dr. Karyn Baum, Vice President for System Clinical Operations. “Having access to machine learning that helps us identify patients ready for discharge, patients ready for transfer – those become essential. Qventus gives us eyes on what really matters.”
As M Health Fairview moves towards coexisting with COVID-19 in the medium term, leadership is leveraging real-time scenario planning tools to predict COVID-19 demand, including the impact of social distancing changes and other measures as the pandemic evolves.
This predictive power has allowed M Health Fairview to restore operations and revenues with agility, quickly returning to 85% of their pre-COVID-19 surgical volume and mitigating $30 million per week revenue loss[3] from deferred electives during the surge. Going forward, M Health Fairview is looking to continue its use of machine learning to hardwire discharge optimization and expand the role of predictive analytics to drive operational efficiencies across the health system.
M Health Fairview’s CEO James Hereford describes the balancing of near-term crisis management with longer-term value creation this way.
“With Qventus, we’re empowering teams across different levels of the organization to work together as a truly integrated system so that we can deliver quality care and drive efficient patient flow. As we navigate the longer-term impact of COVID-19, we look forward to building on our successes with Qventus to further create sustained virtual capacity and maximize our existing system resources.” —James Hereford, CEO, M Health Fairview
Qventus has enabled M Health Fairview to
- Give Incident Command Center visibility into negative airflow, ventilator, and ICU resources – in just days.
- Create “virtual” capacity without adding staff, using AI to unlock ICU and Med-Surg capacity across facilities.
- Decrease length of stay and operating costs, while delivering quality care, through automated operations.
Now and Forever
Although often attributed to Albert Einstein, California Senator Dianne Feinstein noted in a 1985 interview that when playing a new game, “you have to learn the rules and play it better than anyone else.”[4] Spurred by COVID-19, the pace of disruption roiling U.S. healthcare is accelerating.
Enlighted health systems like M Health Fairview are using technology to enhance the performance of their frontline personnel and expand capacity during the pandemic. M Health Fairview is able to respond, act, and win because of their initial foundation of operational excellence, as well as their appetite for moving quickly and adapting to new rules of the game.
In doing so, the system is advancing more efficient, higher-volume, patient-centric care. Moreover, addressing the near-term COVID-19 crisis through real-time operations creates organizational capabilities that will differentiate M Health Fairview longer term in a post-reform marketplace that rewards high-value health companies.
So the new game is on. Now and forever, healthcare delivery has changed. Budget pressures, customer demands and consumerism will no longer tolerate the old model’s inefficiencies and waste. There will be winners and losers. For agile health systems, it’s time to learn the new game’s rules, play hard and win for patients and communities.
Sources
- https://hbr.org/2020/06/how-one-health-system-is-transforming-in-response-to-covid-19
- https://www.4sighthealth.com/unrelenting-margin-pressures-overcoming-healthcares-softening-revenues-and-rising-expenses/
- https://minnesota.cbslocal.com/2020/04/22/coronavirus-in-minnesota-m-health-fairview-reassessing-if-it-can-perform-elective-surgeries/
- https://www.theguardian.com/commentisfree/2016/apr/22/internet-criticized-things-never-said-retweets-origin-meme
Co-Author
 Mudit Garg is the CEO and Co-Founder of Qventus, the first AI-based healthcare operations platform for hospitals and health systems. Prior to Qventus, Mudit co-founded multiple technology companies including Vdopia and Hive. He also spent time in McKinsey & Company’s healthcare practice helping large providers with organizational transformation and performance improvement. Mudit has been recognized for leadership as one of the Silicon Valley Business Journal 40 Under 40. He is a Stanford-StartX mentor. He earned his Master’s in Business Administration and Electrical Engineering from Stanford University and a Bachelors degree from the Indian Institute of Technology.
Mudit Garg is the CEO and Co-Founder of Qventus, the first AI-based healthcare operations platform for hospitals and health systems. Prior to Qventus, Mudit co-founded multiple technology companies including Vdopia and Hive. He also spent time in McKinsey & Company’s healthcare practice helping large providers with organizational transformation and performance improvement. Mudit has been recognized for leadership as one of the Silicon Valley Business Journal 40 Under 40. He is a Stanford-StartX mentor. He earned his Master’s in Business Administration and Electrical Engineering from Stanford University and a Bachelors degree from the Indian Institute of Technology.