December 26, 2025
Finding the ROI in SDOH
In a finding that will surprise no one, a new study correlates social determinants of health (SDOH) — now called health-related social needs (HRSNs) — with higher inpatient admissions and emergency room visits.
What the new study does do, however, is tell hospitals and health systems which HRSNs to spend their money on to get the biggest return on their investment (ROI) with ROI being money saved from fewer admissions and trips to the ER. As the healthcare industry shifts from payment for volume to payment for value (eventually), lowering costs will be the biggest driver of revenue and profit margin.
Five health services researchers from Allina Health in Minneapolis did the study, which appeared in JAMA Network Open earlier this month. They looked at a cohort of 166,682 Medicare and Medicaid patients screened for six HRSNs at Allina care sites and whether resolving those HRSNs led to fewer admissions and ER visits.
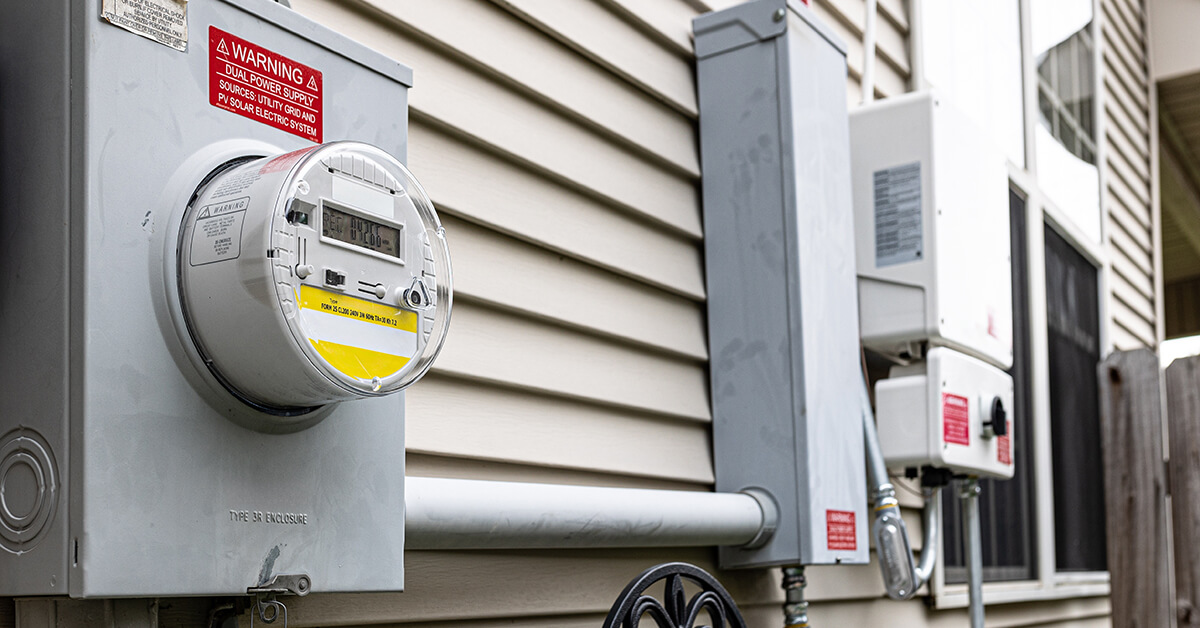
The study period was 2018 to 2022, and the six HRSNs were: housing stability, housing quality, food security, transportation, utilities and interpersonal safety.
Some 24.3% of the patients initially screened for at least one of the six HRSNs with the two highest HRSNs being food security (14.5%) and transportation (8.2%). The two HRSNs with the highest percentage of inpatient admissions were housing stability (10.3%) and transportation (9.5%). The two HRSNs with the highest percentage of ER visits were interpersonal safety (27.7%) and housing stability (26.9%).
The researchers then followed up with a subset of 15,139 of those patients after Allina addressed their respective HRSNs to see if resolution had any effect on inpatient admissions or ER visits six months after resolution.
Turns out, resolving the six HRSNs had no impact on inpatient admissions. None. Zero. Zip. None of the six reduced admissions to any statistically significant amount.
The story was different for ER visits. Resolving four of the six HRSNs — food security, transportation, utilities and interpersonal safety — was positively correlated with fewer ER visits in the six months after the interventions. Two of the six — housing stability and housing quality — had no effect.
So, the bottom line for hospitals and health systems is they can find the biggest ROI for their HRSN spending in food security, transportation, utilities and interpersonal safety on ER visits.
Or, as the researchers put it: “By better understanding how HRSNs are associated with healthcare utilization, health systems can focus their resources on targets that are most meaningful for their patient populations.”
Now let’s see if they do it.
Build a better health system.





