February 17, 2026

Thoughts on the RHTP: What To Do When The Math Doesn’t Math
Since the passing of the One, Big, Beautiful Bill Act of 2025 (OBBBA) and the announcement of the Rural Health Transformation Program (RHTP), I’ve felt a bit like I’m living through George Orwell’s 1984. In the program announcement, Robert F. Kennedy Jr. noted, “This $50 billion program is about delivering dignity and dependable care to rural communities, making sure every American has access to affordable, high-quality treatment.”
And that’s where I get lost. That sounds great, but “affordable, high-quality treatment” requires funding, and as the kids these days would say, “The math doesn’t math.” Let’s take a look:
- Around 20% of Americans live in rural areas and receive care there.
- Those in rural areas have worse health outcomes and are at greater risk of dying from car accidents, suicides, and drug overdoses. Given the role social drivers of health (SDOH) play in our health outcomes, and that poverty, unemployment, lower educational attainment and inadequate transportation are higher in rural areas, these health disparities aren’t a surprise.
- The OBBBA cut ~$900 billion to $1 trillion from Medicaid over 10 years.
- OBBBA also included a fund for rural health transformation, to the tune of $50 billion over five years.
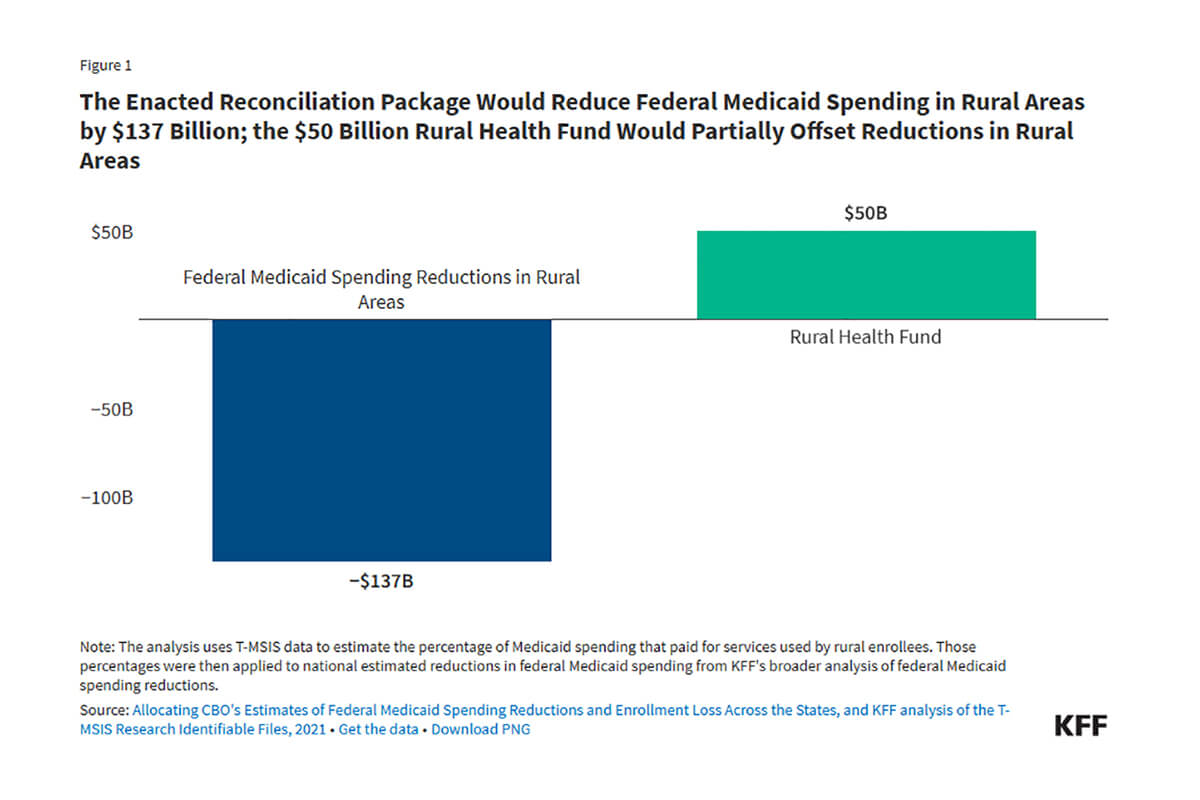
- KFF estimates that Medicaid spending in rural areas will likely decline by $137 billion over 10 years, almost 2.5 times the $50 billion allocated in the RHTP. Becker’s reported that Medicaid cuts will reduce funding in rural environments by $155 billion over the next decade, which is more than 2.5 times the RHTP fund amount.
KFF’s visualization of the net-negative financial impact of the OBBBA on rural health:
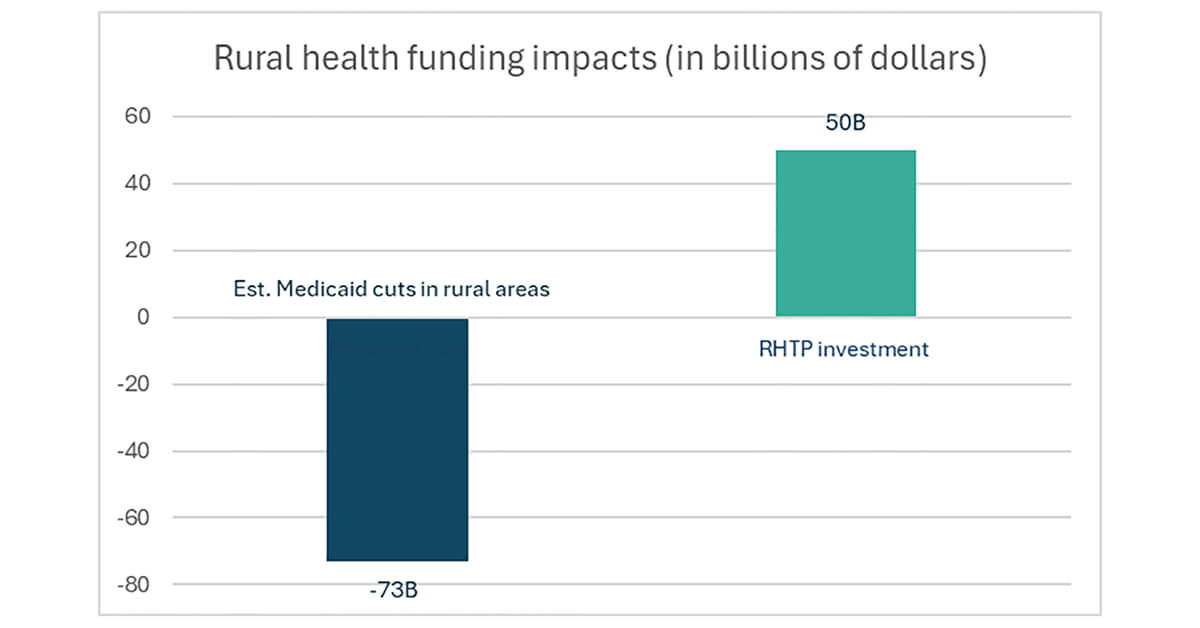
Therefore, I don’t follow how $50 billion over five years (which is awarded to states, not providers) is great or transformative when $137 billion to $155 billion is taken away. Granted, $137 billion to $155 billion is over 10 years, and $50 billion is over five years. So, let’s say $73 billion is for the first five years (my finance professors would disapprove of my oversimplification); that’s almost a 50% reduction. Looking at the numbers on a five-year basis results in the following visual:
Granted, the reduction in Medicaid spending compared to the “investment” in rural health transformation isn’t an apples-to-apples comparison. Medicaid payments go to rural health providers (hospitals, clinics, etc.) and pay providers for care they’ve already provided. Conversely, CMS states that the RHTP will invest in infrastructure to strengthen communities and improve health outcomes.
But how can you improve the infrastructure if it crumbles due to insolvency? This is where I conclude that I must be missing something…
What Am I Missing?
Well-respected thought leaders and analysts have pointed out that the RHTP may embody the same benefits we saw from the $30 billion HITECH Act that pushed healthcare from paper to electronic records (one example here). I’d argue there are also downsides of HITECH, including less face-to-face time between providers and patients and an increase in physician burnout. But I digress…
Leading thinkers beyond those linked above rightly point out that this is a major opportunity for digital health companies. Still, I wonder if that will translate to effective deployment of digital health solutions in rural populations. Depending on the context someone is living in, they may be unlikely to “hire” a digital health offering. Might RHTP help digital health companies? Absolutely. But will it help rural inhabitants? That remains to be seen. As Christina Farr rightly points out, “the devil is in the details.”
I tend to align more with the thinking shared by ER doctor Sophia Spadafore, if for no other reason than it makes financial sense. If ~20% of ER visits go unpaid, this number will only increase in an era when 10 million fewer people are insured, and Medicaid funding has been slashed. If ERs don’t get paid, they can’t function or provide care.
To be clear, we should be investing more upstream in primary care and more drivers of health-oriented solutions (see here and here for how we could do that as a country), but it’s not clear to me how the RHTP will execute on such a shift.
It’s not that reallocating funding toward upstream interventions and the infrastructure to improve health is a bad thing. It’s not. It’s a great thing. DOH research highlights that only 10-20% of outcomes are related to medical care (see graphic below).
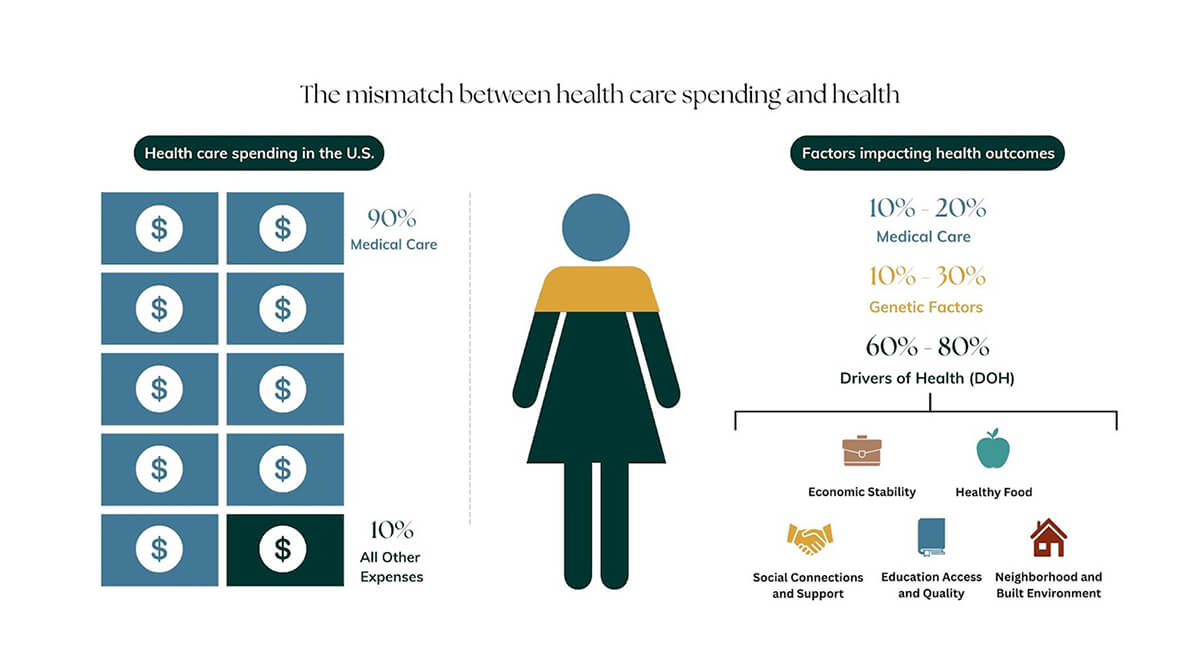
But it’s unclear how (if at all) this $50 billion will be used to support other DOH, such as the built environment, enhanced social support, access to nutritious foods, better education, etc. And after all, those are the levers we need to pull if we truly hope to improve health in rural populations.
So, I’m stuck. I can’t compute (pun intended) how reducing rural health spending will improve health.
What Do You Think? Where Are My Blind Spots?
I need input on three questions to help me see what I can’t figure out:
- From your point of view in the healthcare industry, will the RHTP be a net-positive or net-negative for health outcomes in this country over the next 10 years?
- Which aspects of the health and healthcare industries do you think will benefit most from the RHTP?
- Who will be the biggest losers in the RHTP, and how will those losses be offset in terms of health gains?
I know many people don’t like to share their thoughts in the comments, and that’s okay. I welcome all feedback via email. I read all of your messages and hope many of you will chime in.




