March 26, 2020
Pandemic Preparedness 101: Creating Appropriate Surge Capacity

St. Peter’s Hospital, Helena, MT, 3/18/2020. Photo Credit: Brandi Lyon Photography / Shutterstock.com
In 2014, Israel opened a parking garage that can be turned transformer-like into a 2,000-bed hospital.
The architects hired by the Rambam Medical Center in Haifa designed the walls of a 1,400-car underground garage to include and store pull-out beds, oxygen tanks, dialysis machines, medical supplies and all the other equipment needed to convert the three-story facility into an emergency hospital. It has its own back-up electricity generator and, in a pinch, can provide almost every hospital and surgical service offered in its main buildings.
For a nation like Israel that faces the constant threat of missile, military and terrorist attacks, not to mention global pandemics like the current coronavirus outbreak, investing in hospital-surge capacity seemed a small price to pay to assure that healthcare services would be available to everyone who needs them in an emergency. The never-used $150 million facility requires routine inspections and maintenance to insure all its drugs and supplies are up to date and its equipment is in working order.
The coronavirus/COVID-19 pandemic has exposed the American hospital sector’s woeful lack of preparedness for sudden surge in demand. Frontline hospital workers are in a desperate scramble to obtain coronavirus test kits and an adequate supply of ventilators, face masks and personal protective equipment. Even as the pandemic unfolds, government and healthcare system officials need to explain why they failed to stockpile these crucial supplies and maintain a domestic industrial base capable of resupplying them.
Those are not the only shortages we face. With intensive care units in a few large cities quickly filling to capacity and hospitals scrambling to free up space by cancelling elective surgeries, it’s become abundantly clear that the physical capacity of the nation’s hospital sector also isn’t up to the task of caring for people during a deadly and widespread infectious disease outbreak. Public health researchers at Harvard University project four out of every five patients needing ventilation and ICU care won’t find beds in a worst-case scenario, one where 40% of the population contracted COVID-19 over the next six months.[1] Perhaps someone should print that on t-shirts and hand them out to college students still partying on southern beaches.
We don’t need to build more beds. The U.S. would have been better prepared if we had the right kind of beds.
It’s not as if the nation hadn’t gone through a series of crises over the past quarter century that raised the alarm about the lack of emergency preparedness in the healthcare sector. There were local disasters like the Oklahoma City bombing in 1995 and numerous mass shooting incidents. There were national threats ranging from the anthrax scare after 9/11 to multiple pandemic alerts beginning with the SARS outbreak in 2003.
As recently as 2017-18, the worst annual influenza pandemic in a decade took over 60,000 lives and taxed the hospital sector to its limits. Yet other than a few healthcare policy wonks, does anyone even remember hearing about it? In the midst of that outbreak, the Trump administration – with barely a ripple of protest – dismantled the White House’s National Security Council Directorate for Global Health Security and Biodefense, set up in 2014 after the Ebola outbreak.
“I was mystified when the White House dissolved the office,” Beth Cameron, its last director, wrote in the Washington Post. “The job of a White House pandemics office would have been to get ahead: to accelerate the response, empower experts, anticipate failures, and act quickly and transparently to solve problems.”[2]
But even a transparent and well-functioning federal response to the latest outbreak would have been incapable of correcting the shortage in surge capacity, which is the product of decades of neglect by policymakers. Former White House chief of staff Rahm Emanuel famously said during the 2009 financial meltdown, “You never want a serious crisis to go to waste.” Yet, when it comes to public health crises, we did. Time after time.
Now, with the U.S. in the throes of a full-scale coronavirus panic and much of the nation on lockdown, healthcare providers’ immediate agenda calls for federal policymakers to rectify the disheartening shortages of vital tests and equipment. But with the economy in freefall and Congress contemplating a $2 trillion corporate and individual relief measure, they should also tell Congress to begin preparing for future pandemics. The stimulus bill needs to include funds to rebuild America’s hospital sector so it will be ready for the next big one.
An Appropriate Stimulus Plan
Recent interviews with hospital planners, architects and designers suggest a fifth of beds in the nation’s community hospitals could be rebuilt for surge readiness with a $75 billion grant and loan program. The principles for such a program – a modern-day reworking of the 1946 Hill Burton Act[3] that flooded communities with grants and loans to expand hospital capacity – are straightforward.
First, the program needs to rebuild and reconfigure a meaningful share of existing hospital bed capacity to serve multiple purposes. In an emergency, some portion of standard rooms in the hospital must be convertible into ER and intensive care beds. The American Hospital Association’s most recent survey of the nation’s 5,400 hospitals revealed there are less than 69,000 intensive care unit beds available for U.S. adults.[4] Other estimates put the total as high as 85,000.
Either number is far below what the U.S. needs during a nationwide infectious disease outbreak. The Harvard researchers estimated that under a middle-case scenario – where the infection curve is spread over a year – the U.S. would still need three times more ICU beds than it has now. Regular hospital capacity would be close to adequate as long as local officials emptied half of current occupancy by postponing elective surgeries. Therefore, the strategy for the rebuilding program should be to rebuild and re-equip some portion of existing rooms so they can be used as ICU beds in an emergency.
Second, the government can’t allow hospitals to use the funds for capacity expansion. Advancing technology and patient preference is moving care to home and outpatient settings. This will accelerate after the current crisis without government help. Providers’ wider use of telehealth to analyze and offer treatment to those with mild symptoms of Covid-19 is educating a broad swath of the public about the potential to use this technology for routine care.
The program can accelerate these trends by helping providers build outpatient facilities that can be rapidly converted into hospital beds, even as they shrink traditional hospital capacity. Meanwhile, hospitals in growing markets can tap existing financing tools for needed expansion projects, not the emergency preparedness fund.
Third, the new program should pay special attention to the needs of rural, small city and critical-access hospitals. The healthcare needs of towns with aging, shrinking populations have changed dramatically from the days when their hospitals were built.
Those hospitals need a special infusion of cash to redesign their facilities to meet current needs while installing emergency surge capacity.
Fourth, emergency rooms should be rebuilt and reconfigured so they can rapidly change into isolation and triage centers for infectious disease patients. Tents in parking lots or on hospital lawns are not the appropriate solution. Experts say ER procedures during an outbreak need to follow normal routines as closely as possible to protect emergency medical technicians, frontline hospital workers and their patients from the unnecessary spread of disease. That’s best done in a permanent facility.
Very few hospitals across the country have moved to make these investments on their own. “I don’t see a lot of money being put into it,” says Cyndi McCullough, director of evidence-based design at HDR, the nation’s largest hospital architecture-design firm. “Most budgets don’t accommodate planning for surge.”
Rush University Medical Center is among the early movers. It incorporated surge capacity into the design of its new 700-bed hospital in Chicago’s near West Side, which was built in 2012. Its chief concerns in the mid-2000s, when planning for the new facility began, were major bioterrorism incidents or a pandemic like the one we’re going through now.
“A lot of things were built in,” says Dr. Anthony Perry, vice president for ambulatory transformation at Rush and the lead clinician involved in the project. “How the ER expands outside the walls of the hospital to do forward triage and decontamination; how the ER surges to triple its capacity if need be; how we manage air handling across the facility; how we isolate people if they have something infectious. The work was in doing it smartly rather than spending more money.”
In a quarter of its rooms in the main wings of the hospital, Rush installed sophisticated air-handling controls that can quickly convert rooms with everyday airflow into negative pressure rooms that can isolate patients and prevent the spread of infection.
Perry emphasized the need for regional planning when deciding major new investment in surge preparedness. “Does every hospital need to go through pandemic preparedness? Assuredly not. We’re a healthcare facility that works with other facilities in Chicago. We’re part of the bioterrorism response network. Everyone needs to figure out what their role is going to be.”
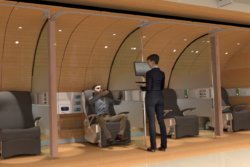 HKS designed a special area at the Northwestern Hospital Emergency Department for patients to be examined and treated in highly space efficient ‘Pods’ intended for surge capacity to cohort patients during the flu season. The pods have infection control in mind with highly cleanable surfaces, protected equipment to avoid cross contamination and speed up effective cleaning between patients. And the pods have patient amenities more normally associated with airline first class accommodations than an emergency department exam/treatment space. Northwestern ED has 16 pods in the same space as 4 traditional exam rooms.
HKS designed a special area at the Northwestern Hospital Emergency Department for patients to be examined and treated in highly space efficient ‘Pods’ intended for surge capacity to cohort patients during the flu season. The pods have infection control in mind with highly cleanable surfaces, protected equipment to avoid cross contamination and speed up effective cleaning between patients. And the pods have patient amenities more normally associated with airline first class accommodations than an emergency department exam/treatment space. Northwestern ED has 16 pods in the same space as 4 traditional exam rooms.
A Bearable Cost
Building greenfield surge capacity is out of the question. Estimates for new hospital construction range as high as $2 million per room if you include all the ancillary space like the ER, nursing stations, pharmacy, utilities, supply closets and offices.
Retrofitting rooms and facilities to serve multiple purposes won’t be cheap, but it’s affordable, especially when stacked up alongside the forthcoming stimulus plan. Remodeling standard single rooms in an existing hospital so they could be rapidly turned into double-occupancy ICU rooms during a pandemic would cost, on average across the country, about $750,000 per room. That’s according to rough estimates provided by David Vincent, a senior planner and principal at HKS, one of the nation’s leading hospital architecture firms.
Here’s a hypothetical project. Take a 250-bed community hospital that typically operates at about 60% of capacity. It has a 25-bed ICU unit. Its planners’ projections, given the ongoing movement toward one-day procedures and outpatient services, show a 200-bed hospital would serve the community’s needs. With government funding, its owners could do a gut rehab of 100 rooms that replaced them with 50 spacious and attractively designed single-occupancy rooms that have all the air, utility and gas hook-ups necessary to rapidly convert them into 50 double- occupancy ICU-style rooms (100 beds) during a pandemic or mass casualty incident. Total cost? About $37.5 million.
“After 9/11, there was a lot of talk about building for surge,” Vincent says. “I lived that for four years when talking about projects and saw almost none of that happen. (He’s referring to ER One, the prototype for a surge ready emergency care facility developed at Washington Hospital Center in Washington, D.C. [5]) Good ideas are out there. And it’s a good buy.”
So why doesn’t it happen? “I can only think the margins on these hospitals are so thin that they say we can only go with what we have to have, and not what is the right thing to have,” Vincent says.
That’s why only a Hill-Burton-style federal program using grants and no interest loans can make it happen. House and Senate leaders are considering a $2 trillion economic stimulus package to rescue the U.S. economy from the fallout from our current unpreparedness. Earmarking $75 billion for a five-year, job-creating construction program could transform 20% of America’s hospital rooms into potential surge capacity, even as it shrank that capacity during normal times to better meet the nation’s changing demand for routine hospital care.
Last week, I ran the idea past Rick Pollack, CEO of the American Hospital Association. He called it the “phase four” of the nation’s crisis response. The first phase focused on developing tests and getting them out into the field, he says. The second focused on getting financial aid for hospitals, caregivers and individuals without insurance coverage. The third, now under discussion, will, in addition to the economic bailout, include beefing up the supply chain for much-needed ventilators, masks and other personal protective equipment and helping hospital develop surge capacity from what they’ve got, whether in existing facilities or putting tents in parking lots.
“After every experience you learn,” he says. “What’s odd about this is that we also must face the pressures on us to cut costs and move things out of the buildings. Most capital projects are designed to build in more cost effectiveness. What may be required is to rebuild and prepare better for the future.”
Key Takeaways
- The $2 trillion COVID-19 stimulus plan represents a golden opportunity to help the hospital sector expand much-needed surge capacity.
- Up to a fifth of US hospital capacity should be retrofitted for dual use: modern single-occupancy rooms that can change into double occupancy ICU rooms in an emergency.
- A well-designed program would dovetail neatly with more care moving from in-patient to out-patient settings.
- About $75 billion in grants and no-interest loans would get the job done without jeopardizing hospital balance sheets or raising patient and payer costs.
Sources
- Thomas C. Tsai, Benjamin H. Jacobson, Ashish K. Jha, “American Hospital Capacity And Projected Need for COVID-19 Patient Care,” Health Affairs blog, March 17, 2020 (https://www.healthaffairs.org/do/10.1377/hblog20200317.457910/full/, accessed March 20, 2020).
- Beth Cameron, “I ran the White House pandemic office. Trump closed it,” Washington Post, March 13, 2020 (https://www.washingtonpost.com/outlook/nsc-pandemic-office-trump-closed/2020/03/13/a70de09c-6491-11ea-acca-80c22bbee96f_story.html, accessed March 23, 2020).
- The 1946 Hill-Burton Act provided grants and low-interest loans to non-profit hospitals and other healthcare facilities to expand and modernize their facilities.
- American Hospital Association, “Fast Facts on U.S. Hospitals, 2020” (https://www.aha.org/statistics/fast-facts-us-hospitals, accessed March 24, 2020).
- See The Joint Commission, “Surge Hospitals: Providing Safe Care in Emergencies,” 2006 (https://www.jointcommission.org/-/media/deprecated-unorganized/imported-assets/tjc/system-folders/topics-library/surge_hospitalpdf.pdf, accessed March 24, 2020).





