October 22, 2019

A Second Coming: Medical Education’s Desperate Need for Another Flexner Revolution
On June 26th, 2019, American Academic Health Systems announced its intention to cease all medical activities at Hahnemann University Hospital by September 6th, 2019. With roughly 17,000 annual admissions, Hahnemann has been Philadelphia’s fifth largest hospital [1] and the primary teaching hospital for Drexel University College of Medicine.
Hahnemann has a storied 171-year history that includes several regional firsts: first kidney transplant; first Level One trauma center; first and only artificial heart implant. It also has treated many famous patients, including Grace Kelly and Gerald Ford.
In recent decades, Hahnemann has served largely low-income people of color at its gentrifying Center-City location. For this reason, many characterize its closure as valuing money more than people. Presidential candidate Bernie Sanders pounded on this theme during a July 15th, 2019 rally,
“This is not just a Philadelphia issue, it is not a Vermont issue, it is a national issue. If developers can turn the hospital into luxury condos, it will send a signal to every vulture fund on Wall Street that they can do the same thing in community after community.”
The forces driving Hahnemann’s closure, however, are far more nuanced and pervasive than simple greed. Through a coordinated effort, Philadelphia’s other hospitals have absorbed Hahnemann’s patients and residents. After Hahnemann’s closure, there remain ample hospital beds to meet the region’s acute care needs.
In an insightful editorial, the Philadelphia Inquirer described Hahnemann’s closure as symptomatic “of a bigger disease.” High healthcare spending has not improved community-wide health and wellness.
Philadelphia spends as much or more per capita on medical treatment as any city in the country, but suffers declining life expectancy, exceptionally high infant/child mortality and unacceptably low health status. As the Inquirer observed, this dismal reality compromises Philadelphia’s long-term livability
and sustainability.
“A city where more and more people are sicker, leading to an inability to contribute and thrive, strains the system and takes away resources from other vital needs.”

Philadelphia is not unique. American society spends lavishly on healthcare but gets too little in return. In this sense, Hahnemann’s closure reflects medicine’s monumental failure to adapt its training, facilities and services to meet the American people’s true health and wellness needs.
Nowhere is healthcare’s “disease” more prevalent than in the halls of nation’s medical schools and academic medical centers. It’s time to reinvent academic medicine so that it serves consumers, not just science.
With innovation, augmented intelligence, team-based training and transparency, tomorrow’s doctors will become part of a technology-rich, human-centered ecosystem that partners 24/7 with individuals to advance their health and wellness.
A customer revolution is quietly reshaping healthcare. Slow-footed, costly and bureaucratic, academic medicine is ill-prepared for this disruptive revolution. To remain relevant, academic medicine must rediscover its purpose, embrace consumerism and reinvent itself. How many more Hahnemann’s will have to close before academic medicine gets this message?
Academic Medicine’s 19th Century Mindset[2]
This is the second time American medicine has confronted a crisis of conscience. By the early 1900s, the United States had only a few elite medical enterprises that incorporated rigorous training, scientific research and clinical consistency into their operations. The most notable was the then-new Johns Hopkins School of Medicine (founded in 1893).
In contrast, the vast majority of medical organizations at that time were squalid, unregulated, clinically inadequate and staffed by quacks. With the support of the American Medical Association, the Carnegie Foundation engaged Abraham Flexner in 1908 to survey medical education in the U.S. and Canada. Flexner published his findings in 1910.
The Flexner Report revolutionized American medicine. It called for rigorous admission criteria, adherence to scientific protocols and state regulation of medical organizations. Few medical schools met Flexner’s standards. He recommended closing more than 120 of the 150-plus medical schools then operating in the country.
Response to the Flexner Report was rapid and profound. Within four years, 31 states refused to license graduates from substandard medical schools. Within 10 years, almost a hundred medical schools closed or merged. Despite a fast-growing population, the number of U.S. medical students dropped from 28,000 in 1904 to 14,000 in 1920.
The Flexner Report also promoted the Johns Hopkins training model of medical education: two years of science education and two years of clinical training, followed by extensive residencies at teaching hospitals. Medical schools universally adopted the Hopkins model and operated within a tripartite mission (education, research and clinical practice) that emphasized the power of science and the necessity of academic freedom.

The broad adoption of the Hopkins model modernized American medicine, which emerged as the global leader in medical research and innovation. The tripartite academic model remains largely unchanged from its 19th-century origins. It’s showing its age.
The Hopkins model perpetuates the following practices that contribute to healthcare’s systematic dysfunction and disconnection with consumers. To this day we see that:
- Medical student selection and training emphasize memorization, individual mentoring, hierarchy and full treatment responsibility resting on physicians’ shoulders.
- Doctors learn to distrust information, team dynamics and new treatment methodologies.
- Education and training models perpetuate a rudimentary “see one, do one, teach one” education/practice model.
- Medical education excludes economics, management, communications, creativity and organizational dynamics — areas of expertise that are essential to high-functioning professional organizations.
- Medical practice grants higher status and higher compensation to students pursuing specialty care as opposed to those pursuing primary care. The culture of academic medicine supports this inbred preference for specialized training.
Unchecked, the Hopkins model has created a dramatic oversupply of specialty physicians and facilities and an equally dramatic undersupply and primary care physicians and services. It lends itself to centralized, high-cost campuses, hierarchical management systems, and fragmented depersonalized patient care with unacceptable error rates.
Modern medicine has created a “superstar” physician marketplace that rewards individual achievement and discourages team-oriented behaviors. It lacks standardization, avoids accountability and delivers suboptimal care outcomes.
As a result, American medicine has become a cult the following four catastrophic biases[3]:
- a bias for autonomy;
- a bias for control;
- a bias for hierarchy; and
- a bias against creativity.
These deeply ingrained biases infect medical education to its core and shape medical student selection, medical training, clinical practice and biomedical research.
More of the same is a recipe for disaster. Medicine needs a new “Flexner” revolution that recognizes that the scientific basis for medical education is no longer sufficient. It must deprogram itself to eliminate its counterproductive biases. It needs to train humans to be better humans, not better robots.
American society will not wait forever for medical education to transform itself. Consumers aren’t buying what medicine is selling. Their demands for better health and healthcare services are driving industry transformation.
Healthcare’s Copernicus Moment

In 1543, Polish mathematician and astronomer Nicolaus Copernicus turned the theological and scientific worlds upside down when he posited that the sun, not the earth, was the center of the known universe. Like the Catholic Church in the 1500s, healthcare is coming to terms with a new operating reality: the industry revolves around customers and consumers, not payers, providers and suppliers.
Healthcare consumers, particularly millennials, are becoming more discerning, demanding, tech savvy and impatient. They’re frustrated by poor service and becoming “mad as hell and not willing to take it anymore.” They resent middlemen that drive up prices and stand between them and service providers. They expect easy-to-execute transactions with clear prices.
For example, an individual needing a knee replacement wants to know: how long they’ll be in the hospital; how long it will take to get back to normal activity levels; how much it will cost; and who will pay for unanticipated complications. Consumers expect to compare providers and facilities based on outcomes, price and other patients’ experiences.
In response, innovative health companies are racing to meet consumer demands for better outcomes, service and value. These “revolutionary” companies differentiate themselves through brand strength, price and customer experience. The shift toward full-risk contracting (e.g. bundles, capitation) strengthens their market competitiveness. Adding fuel to the fire, record levels of smart private equity and venture investment are funding their growth.
Amazon divides consumers into millions of segments based on their tastes, buying history and hundreds of other variables. Mirroring Amazon, revolutionary health companies (including some health systems) are embracing consumer segmentation. Through data customization, personalization and communication, Amazon guides consumers to make better health and healthcare decisions. Tech-savvy, they give consumers a single point of contact and create a seamless service experience across.
Medical education programs will have to sprint to keep up with this pace of disruptive change. It’s time to “think different” and proactively pursue institutional transformation. It won’t be easy. Overcoming medicine’s ingrained biases, asset-heavy operating platforms and 19th-century management practices requires a full-fledged commitment to training, triage, technology and teamwork (the 4 T’s).
Training: preparing medical professionals to succeed in consumer-centric business models that reward coordination, transparency, outcomes, consumer engagement and creativity.
Triage: delivering the right care at the right time in the right place at the right price. This will require health systems to decant routine / commodity care from inconvenient, high-cost acute facilities. It also requires enhanced primary care services that meet consumers’ specialized care needs in personalized delivery models.
Technology: recognizing technology is a means, not an end. Consumers want to engage with healthcare the way they engage with other services. Telemedicine will be everywhere. Like banking, medicine will not differentiate between virtual and in-person service delivery.
Importantly, liberated data will flow freely into apps that support consumerism and guide real-time care delivery. Simulation centers, virtual reality and every other tech capability that advances care, reduces friction, lowers costs and enhances customer service will become mainstream.
The myth that there is not enough data is exactly that. Data overwhelms healthcare providers. The challenge is to simply and deeply analyze the data so as to be actionable across many platforms.
Teamwork: adopting team-based solutions that institute a universally high standard of care delivery built on trust, shared information, effective transitions and accountability. Care teams will learn from mistakes and adapt protocols accordingly.
Medical education has the opportunity to reinvent itself by embracing its core values of humanity, humility, curiosity and shared inquiry / problem-solving. It also must adopt its business models, technology and practice patterns to deliver patient- and consumer-centric health and healthcare services.
Failure to do so will cause academic medical enterprises to lose societal relevance and respect. Healthcare’s brave new world is upon us. It’s “adapt or die” time for academic medicine, particularly as the broader industry reinvents itself. Doctors must heal themselves.
Reprogramming Medical Education

The transformation of healthcare delivery must begin by reprogramming medical education and training. Medicine must modernize and reconfigure its practices to advance kinder, smarter and more affordable healthcare services. In particular, it must do the following:
- Select and train medical students to apply technologies that can guide care delivery in real time. Move health equities, communication skills, quality benchmarking, and creative thinking from “soft electives” to the core curriculum.
- Use simulation centers to replicate real-world medical delivery to reduce medical error, standardize operations and facilitate triage. Engage in cross-curricular training among healthcare professionals to develop more effective, team-based delivery models.
- Expand curriculum to teach management, economics and leadership so individual physicians make smarter resource allocation decisions, lead care teams more effectively and accept more-expansive performance monitoring with greater accountability.
- Place less emphasis on on physicians conducting biomedical breakthrough research and greater emphasis on primary care practice, emphasizing disease prevention, patient engagement and health promotion.
- Research the effectiveness of new care delivery models. Incorporate social determinants of health into all aspects of academic medicine (clinical, educational, research).
- Create synergistic opportunities for students and faculty to interact with entrepreneurs and engineers from start-up companies to turbocharge innovation and develop application that advance AI and machine learning technologies.
Digitized data, computational speed, predictive analytics and global connectivity are transforming all human enterprise. Predictive analytics can identify those most at risk for acute episodes and suggest preventive interventions. Head-to-head algorithms consistently make better diagnoses than doctors, but
that is only half the story.
No one expects human beings to outrun cars. Likewise, applications can substantially improve real-time performance of healthcare professionals. Machine-based learning tools work best when combined with human intelligence. Moreover, failure to use proven computational tools “kills” patients through misdiagnosis, mistreatment and mistakes.
It also is essential to develop “team of teams” organizational structures to solve complex medical challenges in real time under dynamic conditions with appropriate data and technological support. The goal is to make it easier and less stressful for clinicians to make the right medical decisions in real time.
Academic medicine is notoriously slow to change. The Hopkins model continues to dominate medical education, but there are many promising initiatives occurring in medical education. The medical school Thomas Jefferson University has merged with the art and design school Philadelphia University to introduce more creativity, design thinking and innovation into medical education.
Rutgers New Jersey Medical School combines holistic educational training with on-the-job training to develop highly skilled and compassionate physicians centered on patient needs. Rosalind Franklin University engenders interdisciplinary exchange, research and learning across five professional health schools.

The Icahn School of Medicine at Mount Sinai offers “Nexus Learning” to first- and second-year medical students. Nexus Learning addresses topical policy issues such as harm reduction, advocacy and high value care, all in relation to health promotion, research and delivery. In Focus immersive courses enable students to pursue education in topics related to medical practice and biomedical research. Coursework addresses health disparities locally in East Harlem and throughout the developing world.
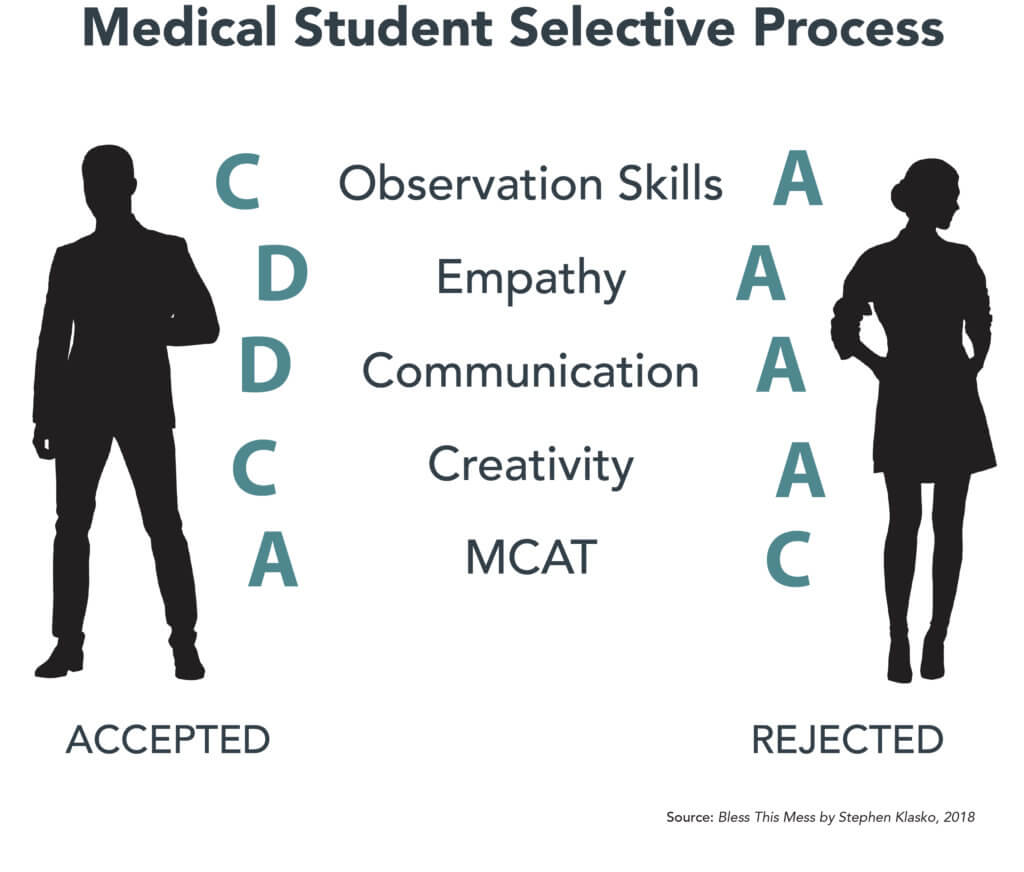
Now in its 12th year, the University of South Florida’s SELECT program (Scholarly Emphasis. Leadership Experiences. Collaborative Training.) emphasizes self-awareness, empathy and communication skills more than memorization and MCAT scores when choosing future medical leaders. Training includes clinical education on-site at the Lehigh Valley Health Network in Allentown, Pennsylvania. SELECT’s holistic philosophy shapes its curriculum in powerful ways.
“The founding principle of SELECT is the concept that students with high emotional intelligence are more likely to develop the skills needed to transform health care and improve the health of communities. In essence: students with a strong foundation in emotional intelligence will become more engaged, compassionate physicians who will connect deeply with their patients and their patients’ families; feel more comfortable with and be more effective as team leaders and team members; and have the relationship building skills and systems perspectives to more effectively lead change in health care organizations.”
As science fiction writer William Gibson famously noted, “The future is already here. It’s just not very evenly distributed.” Bold redesign initiatives like those being undertaken by Jefferson, Mt. Sinai, Rosalind Franklin, Rutgers and USF will redefine medical education and revolutionize academic medicine.
Conclusion: Academic Medicine’s Existential Crisis
Enterprising academic enterprises are challenging every facet of academic medicine with the triple aim of putting consumers first, improving outcomes and delivering value. They’re planning for the future, not repeating past mistakes. They’re engaging customers in their health and wellness. They’re emphasizing care outside the hospital’s four walls. They believe in transparency.
They are making healthcare access more equitable and affordable. They are reinforcing healthcare’s porous primary care defenses to address disparities in social determinants of health. They are building healthier and more productive communities one individual at a time.
To accomplish this, they are advancing consumer-first business models that run high-octane preventive, behavioral and disease management services. In these revolutionary companies, population health and personalized medicine come together. Individuals partner with their health companies to pursue strategies for healthier, happier and more productive living.
Healthcare’s brave new world will reward organizations with the courage to embrace revolutionary change, and it will devour those who fight it. Imagine if everyone who loves academic medicine mirrored Ghandi and became the change they wanted to see in healthcare. Sacred cows would become hamburger.
Lack of imagination may be academic medicine’s principal challenge. Here’s how to overcome this obstacle.
- Identify what will be obvious in ten years and do it now.
- Select and train doctors who are tech-savvy, compassionate, great communicators and team players.
- Use telemedicine, simulation (including virtual reality) and apps to reinvent medical training and care delivery everywhere, including the home.
- Have crucial conversations with these future (and current) physicians and nurses as to why healthcare has not joined the consumer revolution and what we can do about it.
Most importantly, medical education institutions need to make creativity and humanities “required” courses for aspiring doctors and nurses. The world will not end if there is two weeks less of microbiology, pharmacology and anatomy. Programs should use this critical “found” time for improv classes that hone listening and communication skills, for art classes that enhance observation skills, and for collaborative negotiation exercises that enhance real-world effectiveness.
To revolutionize itself, academic medicine institutions must apply the same passion it has for curing disease to curing America’s “very sick” healthcare system. Abraham Flexner would expect nothing less!
Sources
- https://www.inquirer.com/health/hahnemann-temple-patients-er-20190723.html
- The Great Influenza, Chapter 5, by John M. Barry
- Source: Bless This Mess by Stephen K. Klasko
Co-Author
 Dr. Stephen K. Klasko is a transformative leader and advocate for a revolution in our systems of healthcare and higher education. His 2018 book is titled, Bless This Mess: A Picture Story of Healthcare in America – an account of how the USA was elected to the Intergalactic Council of Cool Health Systems by 2035. As President of Philadelphia-based Thomas Jefferson University and CEO of Jefferson Health, since 2013 he has steered one of the nation’s fastest growing academic health institutions with a program based on his vision of re-imagining health care and higher education. His 2017 merger of Thomas Jefferson University with Philadelphia University creates a pre-eminent professional university that includes top-20 programs in fashion and design, coupled with the first design thinking curriculum in a medical school, and with the nation’s leading research on empathy. More info here.
Dr. Stephen K. Klasko is a transformative leader and advocate for a revolution in our systems of healthcare and higher education. His 2018 book is titled, Bless This Mess: A Picture Story of Healthcare in America – an account of how the USA was elected to the Intergalactic Council of Cool Health Systems by 2035. As President of Philadelphia-based Thomas Jefferson University and CEO of Jefferson Health, since 2013 he has steered one of the nation’s fastest growing academic health institutions with a program based on his vision of re-imagining health care and higher education. His 2017 merger of Thomas Jefferson University with Philadelphia University creates a pre-eminent professional university that includes top-20 programs in fashion and design, coupled with the first design thinking curriculum in a medical school, and with the nation’s leading research on empathy. More info here.
Outcomes Matter. Customers Count. Value Rules.
Join The Customer Revolution in Healthcare!
Read about today’s revolutionary forces and leaders in The Customer Revolution in Healthcare, available for purchase on RevolutionaryHCare.com.





